What are the key considerations in the debate around assisted dying/assisted suicide?
A summary of our inquiry

Introduction
In December 2022 we launched an inquiry to examine different perspectives in the debate on assisted dying/assisted suicide. We wanted to deepen our understanding of the broad range of views on this topic and to examine evidence from jurisdictions where this practice is legal. We set out to produce a report which would act as a comprehensive basis for future debate in either House of Parliament. To do this, we:
- asked for written submissions in response to the terms of reference for the inquiry
- heard from experts during oral evidence sessions, which are recorded on parliamentlive.tv
- asked members of the public to share their views in an anonymous online public engagement form
- visited health professionals in Portland, Oregon to deepen our understanding of the topic
- visited the Royal Trinity Hospice in Clapham, South London
Throughout the inquiry we published:
- transcripts of public meetings
- a full thematic analysis of responses to our online public engagement form
- a full report of the evidence gathered throughout our inquiry
Here, we have summarised what we did throughout the inquiry.
Read on to learn more.
Safeguarding and support
If you have immediate concerns about yourself or someone else, you should contact the Police on 999. In addition to your GP, the following organisations may be able to offer support or further information:
Samaritans: Support and guidance for everyone. Call 116 123 - 24 hours a day every day or email jo@samaritans.org.
The Silver Line: Support for older people; a free confidential helpline providing "information, friendship and advice" to people aged 55 and over, and support for "older people who are suffering abuse and neglect"; open 24 hours a day every day. Call 0800 4 70 80 90.
Mind: For information, advice, and support for anyone experiencing a mental health problem. Call 0300 123 3393.
How inquiries work
UK Parliament select committees are set up to look closely at different topics and scrutinise the work of government. Committee investigations, called inquiries, deepen understanding of an issue and provide opportunities for members of the public and experts to share their views.
Our inquiry

We collected 389 pieces of written evidence pieces of written evidence
We spoke to members of the public and experts at a roundtable event
We visited Portland, Oregon to learn more about views across the debate on Assisted Dying/Assisted Suicide in place where a form of this practice is legal, introduced by the Death with Dignity Act (1997).
We visited Royal Trinity Hospice, South London, to further understand what can be done to improve palliative care.
We reviewed more than 68,000 submissions to our online public engagement form.
We heard from 20 witnesses during oral evidence sessions
Tuesday 28 March
- Baroness Finlay of Llandaff
- Rt Hon. the Lord Falconer of Thoroton
- Baroness Meacher
- Baroness Hollins
- Dr Naomi Richards, Senior Lecturer in Social Science and Director of the Glasgow End of Life Studies Group at University of Glasgow
- Dr Alexandra Mullock, Senior Lecturer in Healthcare Law and Co-Director of the Centre for Social Ethics and Policy at University of Manchester
- Professor Nancy Preston, Professor of Supportive and Palliative Care at University of Lancaster
Tuesday 16 May
- The Hon Kyam Maher MLC, Minister for Aboriginal Affairs, Attorney-General, and Minister for Industrial Relations and Public Sector at Government of South Australia
- Professor Brian Owler, Consultant Neurosurgeon at the Children’s Hospital at Westmead, the Sydney Adventist Hospital, Norwest Private Hospital and Westmead Private Hospital
- Dr Gary Gheung, Associate Professor & Old Age Psychiatrist, Department of Psychological Medicine at University of Auckland
- Professor Roderick MacLeod, former Senior Consultant and Senior Medical Specialist in Palliative Care
- Dr Chandana Banerjee, Associate Professor Hospice & Palliative Medicine at City of Hope National Medical Center
- Dr Lydia Dugdale, Director, Center for Clinical Medical Ethics, Columbia Vagelos College of Physicians & Surgeons at Columbia University
Tuesday 6 June
- Professor Irene Tuffrey-Wijne, Professor of Intellectual Disability and Palliative Care at Kingston University London
- Professor Jan L Bernheim, Oncologist, Emeritus Professor of medicine and medical ethics, End of-Life Care Research Group at Vrije Universiteit Brussels
- Professor Rutger Jan van der Gaag, Professor of Psychosomatic Medicine and Psychotherapy, Emeritus Professor of Psychiatry and former President at Royal Dutch Medical Association
- Professor James Downar, Professor and Head, Division of Palliative Care at University of Ottawa
- Professor Trudo Lemmens, Professor and Scholl Chair in Health Law and Policy, Faculty of Law at University of Toronto
- Dr Scott Kim, Adjunct Professor Psychiatry, University of Michigan; Senior Investigator at Department of Bioethics at National Institutes of Health USA
Tuesday 27 June
- Dr Georg Bosshard, Practicing geriatrician and nursing home physician, reader for clinical ethics at University of Zürich
- Dr Yvonne Gilli, President at Swiss Medical Association (FMH)
- Professor Samia Hurst-Majno, Professor of Biomedical Ethics at University of Geneva, and member of the Swiss National Advisory Commission on Biomedical Ethics
- Silvan Luley, Team member at DIGNITAS - To live with dignity - To die with dignity
- Bernhard Sutter, Director at EXIT (Deutsche Schweiz)
Tuesday 4 July
- Dr Paul Perkins, Chief Medical Director at Sue Ryder
- Dr Matthew Doré, Honorary Secretary at Association for Palliative Medicine of Great Britain and Ireland
- Jonathan Ellis, Director of Policy, Advocacy & Clinical Programmes at Hospice UK
- Helen Whately MP, Minister of State at Department of Health and Social Care
- Professor Stephen Powis, National Medical Director at NHS England
Read on to learn more
Findings from online submissions

Suicide and attempted suicide are not crimes in England and Wales. However, it is a crime for a person to encourage or assist the suicide of another person. Euthanasia (healthcare professionals administering lethal drugs) is also illegal.
We asked respondents to our online public engagement form if they broadly agree or disagree with current law on assisted dying/assisted suicide and why.
We then asked which three factors from a list of eight influenced their views most and gave respondents an opportunity to share why they selected those options.
The written responses were analysed thematically which involves identifying themes and then counting mentions of those themes across the data collected.
The responses received are likely to demonstrate ‘self-selection’ or ‘volunteer’ bias, meaning they overrepresent people who have high levels of interest in this issue. The findings reflect the key perspectives of those responding and should not be interpreted as representative of all individuals.
Respondents who broadly agree with the current law in England and Wales
Seven themes emerged from the written responses from people who broadly agree with current law on this issue in England and Wales:
- impact on vulnerable groups
- impact on societal perceptions of disability
- potential expansion of eligibility criteria and international comparisons
- access to and impact on palliative and end of life care
- impact on healthcare systems and healthcare professionals
- sanctity of life
- suicide prevention
Overall, the responses focused on the impact a change in the law could have on vulnerable groups and the healthcare professionals who would need to be involved in such a process. Some respondents prioritised this impact over the views of pressure groups and members of the general public who would support a change in the law. Views of religious groups were also raised within some of these submissions.
Many respondents proposed an increase in funding and provision for palliative and end of life care to reduce suffering. They argued that the current law should remain and some felt that further consideration of this issue by the UK Parliament was unnecessary.
Key factors influencing views of respondents who broadly agree with the current law in England and Wales
1. Risk of coercion to vulnerable groups
66% of respondents who said that they broadly agree with the current law in England and Wales
2. Risk of devaluing lives of specific groups
56% of respondents who said that they broadly agree with the current law in England and Wales
3. Sanctity of life
53% of respondents who said that they broadly agree with the current law in England and Wales
Respondents who broadly disagree with the current law in England and Wales
The written responses from those who broadly disagree with the law on this issue also produced seven themes:
- what a change in the law should permit and eligibility criteria
- reducing suffering and improving the experiences of people dying and their families
- personal autonomy and dignity
- access to and limits of palliative and end of life care
- inequalities in the current law
- safeguards and international comparisons
- impact on healthcare systems and healthcare professionals
Generally, these responses emphasised the importance of voices of people with terminal illness and their families. Respondents felt that the views of healthcare professionals and experts should also be considered.
Many argued that a change in the law would require a cross-party approach and, importantly, that the UK Parliament would need sufficient time to consider how such a change would work in practice. Some respondents suggested that parliamentarians should be allowed to vote on this issue according to their own views and conscience, as opposed to the views of their political party.
Key factors influencing views of respondents who broadly disagree with the current law in England and Wales
1. Reducing suffering
94% of respondents who said that they broadly disagree with the current law in England and Wales
2. Personal dignity
86% of respondents who said that they broadly disagree with the current law in England and Wales
3. Personal autonomy
68% of respondents who said that they broadly disagree with the current law in England and Wales

Photo by Priscilla Du Preez/Unsplash
Photo by Priscilla Du Preez/Unsplash

Photo by Jonas Leupe/Unsplash
Photo by Jonas Leupe/Unsplash

Photo by Daniel Thomas/Unsplash
Photo by Daniel Thomas/Unsplash
Learnings from Portland, Oregon

Our visit to Portland, Oregon
We visited Portland, Oregon to learn more about views across the debate on assisted dying/assisted suicide in place where a form of this practice is legal, introduced by the Death with Dignity Act (1997).
We met people with a range of views on the Act when we visited the Death with Dignity National Centre and met representatives from the campaign group Physicians for Compassionate Care. We also visited the Oregon Health Authority to better understand how the Act was monitored.
We spoke to people who had been involved in the process of introducing the Death With Dignity Act, and we discussed how the Act now operates in practice and the concerns that some people have about it.

Photo by Health and Social Care Committee Team/UK Parliament
Photo by Health and Social Care Committee Team/UK Parliament

Photo by Health and Social Care Committee Team/UK Parliament
Photo by Health and Social Care Committee Team/UK Parliament

Photo by Health and Social Care Committee Team/UK Parliament
Photo by Health and Social Care Committee Team/UK Parliament

Building sign with State of Oregon emblem
Building sign with State of Oregon emblem
Our visit to the Royal Trinity Hospice

In January 2024 we visited a hospice in Clapham, South London. The Royal Trinity Hospice provides services to neighbouring areas, offering care both at the hospice and in the community. During our visit we got a tour of the facilities, and had an opportunity to speak to several of the members of staff.
We thank the staff at Royal Trinity Hospice for hosting us.

Photo by the Health and Social Care Committee
Photo by the Health and Social Care Committee

Photo by the Health and Social Care Committee
Photo by the Health and Social Care Committee

Photo by the Health and Social Care Committee
Photo by the Health and Social Care Committee
Our report

Image: UK Parliament
Image: UK Parliament
"The inquiry on Assisted Dying/Assisted Suicide raised the most complex issues that we as a committee have faced, with strong feelings and opinions in the evidence we heard.
We intend the information and testimony we present in our report today to have a lasting legacy and, as we set out in the initial terms of reference, be a significant and useful resource for future debates on the issue. That could still be during this Parliament of course or after the next General Election.
We’re particularly grateful to those who shared very difficult personal stories. The accounts were enormously helpful to us as we considered the issues involved and I’d like to put my thanks on record."
Steve Brine MP
Chair of the Health and Social Care Committee
Our report is not intended to provide a resolution to the debate but as a useful resource for future debates. In the report, we have discussed:
- Parliament and the current law
- the Government's role in the debate
- international examples of jurisdictions where AD/AS is available in some form
- the involvement of physicians and assessments of eligibility and capacity to give informed consent
- palliative and end-of-life care
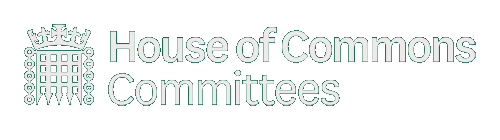
Many of the jurisdictions which have legalised AD/AS did so recently, with still much to learn as time passes. Here, we have captured what we learnt about how this is approached in different contexts:
Elements of this map is informed by the British Medical Association, 'Physician-assisted dying legislation around the world - 1. Map of international jurisdictions' (August 2021). Link: bma-where-is-pad-permitted-internationally-aug-2021.pdf. A full list of sources can be found in the Second Report of the House of Commons Health and Social Care Committee, 'Assisted Dying/Assisted Suicide', Session 2023-24.
Elements of this map is informed by the British Medical Association, 'Physician-assisted dying legislation around the world - 1. Map of international jurisdictions' (August 2021). Link: bma-where-is-pad-permitted-internationally-aug-2021.pdf. A full list of sources can be found in the Second Report of the House of Commons Health and Social Care Committee, 'Assisted Dying/Assisted Suicide', Session 2023-24.
We recommend that the General Medical Council and the British Medical Association develop new guidance to provide clarity to doctors on responding to requests for medical reports for applicants seeking AD/AS abroad.
There was a call for high-quality compassionate end-of-life care across the evidence we received. Another factor highlighted was the importance of agency and control for the person dying.
We recommend the Government ensures universal coverage of palliative and end-of-life services, including hospice care at home, and more specialists in palliative care and end-of-life pain relief.
We are urging the Government to commit to guaranteeing that support will be provided to any hospices which require funding assistance.
Next steps

Our report, 'Assisted Dying/Assisted Suicide', was published on Thursday 29 February, 2024.
The Government has two months to respond.
Thank you to each organisation and each member of the public who contributed to the inquiry, including those taking part in roundtable events.
Before you go...
Cover photo by Priscilla Du Preez/Unsplash